
HOME
 YOUR HISTIO STORY
YOUR HISTIO STORY
I am looking for similarities
in all individual cases of
Histiocytic diseases.
I wonder if we all tell our
stories we might come up
with some commonality
between the specific
situations in which all of
our pets got this disease.
So please email me the
details and I'll put your
pets story on Shelley's
Histio Website
 UW HISTIO VERHAAL
UW HISTIO VERHAAL
Ik ben op zoek naar
overeenkomsten in alle
individuele gevallen van
Histiocytose.
Ik hoop dat wanneer wij
onze Histio verhalen
vertellen, wij overeen-
komsten ontdekken over
de manier waarop onze
huisdieren deze ziekte
hebben opgelopen.
Stuur mij de details en
ik zal het verhaal van uw
huisdier op de Histio
website van Shelley zetten.
 WARNING !
WARNING !
These stories are all
different. Individual
symptoms, situations
and circumstances
may vary and response to
therapy is not always the
same.
- Disclaimer -
 WAARSCHUWING !
WAARSCHUWING !
Deze verhalen zijn allemaal
verschillend. Individuele
symptomen, situaties en
omstandigheden kunnen
verschillen en de reactie
op therapie is niet altijd
hetzelfde.
- Disclaimer -
HISTIOCYTOSIS IN
OTHER LANGUAGES
German - Hund
Maligner Histiozytose
French - Chien
l'Histiocytose Maligne
Italian - Canis
Maligni Histiocytosis
Spanish - Perros
Histiocitosis Maligna
Dutch - Hond
Maligne Histiocytose
HOME
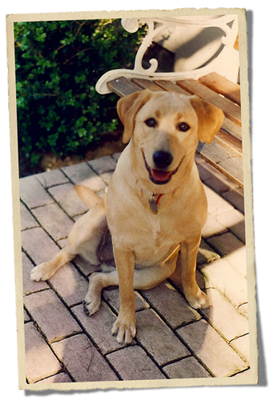
Murphy
Histiocytic Sarcoma
Yellow Labrador Retriever
Female
May 21, 1996 - February 15, 2008


Murphy is the love of my life, the dog I always wanted. When the breeder put that puppy in my arms, we knew we belonged to each other. She was 10 weeks old when she came home with me on August 11, 1996, and she blended perfectly into my life. We became soulmates. I worked full time when she moved in and in less than two months I took a part-time job so I could spend more time with her. She was such a good girl and I wanted to be with her every possible minute I could. My dream was that I would be able to retire and be with her always. I retired in July of 2005.
 Murphy loved all the things typical labs love: eating (especially!), going for walks (which we did every single day, rain or shine, whether I was sick or healthy), swimming, playing, snuggling, sleeping. She had full run of the house and backyard. She slept on my bed and had her place on the sofa, which she loved. When she wanted to snuggle with me on the couch, she'd grab her Nyla-ring and stand and stare at me until I'd say, "Okay, I'm coming," then she'd run and jump into her spot on the sofa where I'd join her later. She was the queen of the castle and of my heart.
Murphy loved all the things typical labs love: eating (especially!), going for walks (which we did every single day, rain or shine, whether I was sick or healthy), swimming, playing, snuggling, sleeping. She had full run of the house and backyard. She slept on my bed and had her place on the sofa, which she loved. When she wanted to snuggle with me on the couch, she'd grab her Nyla-ring and stand and stare at me until I'd say, "Okay, I'm coming," then she'd run and jump into her spot on the sofa where I'd join her later. She was the queen of the castle and of my heart.
Murphy was healthy and happy, loving her life and loving me for 11 years and 9 months. She truly was my life. Everything I did was about her. I never boarded her, always taking her with me on vacations only to places that were dog-friendly. In her entire life, we were apart from each other for maybe two weeks (if you added up the times she had to stay overnight at the vet's and I had to spend the night somewhere else). I always made sure my husband (who lived and worked in another part of the state) was able to come and stay with her at our house when I had to spend the night somewhere else. When Murphy was about three years old, her veterinarian wanted her to lose weight, so I began cooking for her and she lost the weight. I continued cooking her food for the rest of her life. She was an extremely smart and beautiful girl.
February 2003: Murphy was six years old when I discovered a small lump on her right shoulder. Her veterinarian examined it and said it was a fatty tumor and that labs tend to get them. Over the next several years, Murphy continued to develop many, many more of these lipomas. It got to the point where I brought her to the vet about every six months to have them checked. He only palpated them, saying he was sure they were nothing to worry about.
Summer 2007: During the summer of 2007, Murphy developed a slight, infrequent cough, which usually occurred only when I'd come home. She'd be excited to see me and grab a toy, which she always did when anyone came in the door - she'd grab a toy and bring it to you. While the toy (usually a stuffed toy) was in her mouth, she'd cough maybe once or twice, but not all the time. When my husband heard it, he was sure she had a hairball because she did shed a lot and was a good groomer, so we thought hair may have been stuck in her throat.
July 17, 2007: I took her to the vet and asked him about the cough and the fact that when at rest, Murphy's breathing was louder than usual. I had actually brought the loud breathing to his attention quite awhile before. But whenever he'd examine her, he never found anything out of the ordinary. This time he said she had "old dog lung," meaning that typically older dog's lungs lose elasticity and respond to toxins in the air that we all breathe, resulting in louder-sounding breathing.
October 2007: As the months progressed, her cough never improved, so in October, I called to make an appointment with her vet for another check of her lumps and cough. I found out her vet, who cared for Murphy her entire life, had retired and never told his patients! Well, here I must tell you that every time Murphy went to the vet (or even to Petco to get her nails trimmed), she got so incredibly nervous that she trembled like an overgrown Chihuahua! She was inconsolable, shaking and panting as if she was going to pass out or have a massive coronary! It was absolutely frightening to see her like that. So, given that her vet was no longer practicing, I took the opportunity to contact another veterinarian who made housecalls to come over to the house to examine Murphy.
November 7, 2007: The new home-visiting vet came over to check Murphy. He gave her a clean bill of health (her lipomas were okay), but suggested we take her to the Specialty Clinic for a chest x-ray to confirm his suspicion that she had a bronchial infection that was causing her cough.
November 12, 2007: We took Murphy to the Specialty Clinic for her chest x-ray.
Here I have to tell you that I used to pray all the time that Murphy's fatty tumors were confined only to under the skin and that they would all be benign and that tumors would never form in a place that would be dangerous to her health.
Well, the chest x-ray revealed a large tumor in her left caudal lung, confirmed by the radiologist. Our new vet who came to the house said we needed to have that tumor removed as soon as possible and that this would be the best way to not only avoid a potential respiratory emergency, but to get an absolutely accurate biopsy of the tumor.
Because of its outstanding reputation for cutting-edge technology, clinical trials and advancements, as well as having multiple services available in one location, my husband and I decided we wanted to have the surgery done at the University of California at Davis Veterinary Medical Teaching Hospital (an hour's drive from our home) and called to set an appointment for a consultation. They said our consultation would be with an oncologist and the soonest appointment we could get was December 3. The surgery would be even later. Our vet said that was too long to wait and, in fact, withdrew from our case because he didn't want to have to deal with U.C. Davis, which he believed to be too bureaucratic. So, we set up an appointment for Murphy's surgery to be done at the Specialty Clinic where her chest x-rays were done, and her surgery was scheduled for November 19.
November 19, 2007: On the morning of surgery, we (my husband, myself, and a trembling Murphy) met Murphy's surgeon for a pre-surgical consultation. She was an absolute angel - young and extremely knowledgeable, patiently answering each question on my list. She explained that it appeared that Murphy's tumor was a primary lung tumor and it could be benign. The chest x-ray findings indicated no evidence of intrapulmonary metastasis, so she assumed no metastasis had taken place, and if we removed this tumor it was quite possible that all would be well. She even showed us x-rays of another dog who had lung tumors that had metastasized and compared them with Murphy's x-rays, which looked totally different. So, even though I was crying my eyes out during this entire consultation, the surgeon made us feel somewhat confident that removing this tumor would be the answer. We signed all the papers, and the surgeon took my still-trembling Murphy away, but not before I whispered in her ear, "Don't leave me."
 I spent the day trying to keep busy so the hours would pass quickly and Murphy's surgeon called about mid-afternoon. She said Murphy did really well during surgery and that she had removed the entire tumor (including the lung lobe that contained it). She said that Murphy would stay at the hospital over night and most likely the next night. She said we could call the clinic anytime day or night and a doctor would be on duty to speak to us and that we could visit with Murphy the next day and maybe bring her something she would like to eat. Then she told us that she was concerned that while Murphy was undergoing surgery, she noticed that the lymph nodes in her chest were enlarged and that the lymph node tissue looked exactly like the tumor tissue. She said that it was possible that if the pathologist found that the tumor was benign, the lymph nodes could simply be inflamed. We would have to wait for the pathologist's report to be sure what we were dealing with, and that report would be available on November 26.
I spent the day trying to keep busy so the hours would pass quickly and Murphy's surgeon called about mid-afternoon. She said Murphy did really well during surgery and that she had removed the entire tumor (including the lung lobe that contained it). She said that Murphy would stay at the hospital over night and most likely the next night. She said we could call the clinic anytime day or night and a doctor would be on duty to speak to us and that we could visit with Murphy the next day and maybe bring her something she would like to eat. Then she told us that she was concerned that while Murphy was undergoing surgery, she noticed that the lymph nodes in her chest were enlarged and that the lymph node tissue looked exactly like the tumor tissue. She said that it was possible that if the pathologist found that the tumor was benign, the lymph nodes could simply be inflamed. We would have to wait for the pathologist's report to be sure what we were dealing with, and that report would be available on November 26.
I called and spoke with the attending physician at around 8 p.m. to ask how Murphy was doing and he said she was doing fine and to rest assured that he would call during the night if anything was wrong.
November 20, 2007: We visited with Murphy in the early afternoon and brought her a little of her food, which she ate. We were so lucky that she did so well after her surgery that we were able to bring her home at 7 p.m. She ate a little light dinner and we had set up sleeping bags and a mattress on the living room floor so my husband and I could sleep on the floor with her to keep her from wanting to jump up on either the bed or the couch. She was still a bit loopy from the anesthetic and other pain medication she was on (fentanyl transdermal patch), but after a few hours, she settled down and we slept pretty well on the floor through the rest of the night. (Note: The hospital sent us home with Rimadyl, which we started the next day and continued giving to her.)
November 22-25, 2007: Murphy's recovery from this surgery was unbelievable. She wanted so much for her life to be back to normal and she made it so. No one could believe how a dog who had gone through that kind of major surgery could bounce back so quickly. We had canceled all our prior Thanksgiving plans and we celebrated Thanksgiving at home, just my husband, me, and Murphy, with so much to be thankful for - she hadn't left me - she was here! We were so lucky and blessed.
The rest of that holiday weekend was so great. We all moved back into our normal bed at night and Murphy was able to jump back up on the couch and into her favorite spot for TV-watching in the evening. And she was wearing a very cute t-shirt to protect her very large incision. The best news was that since her surgery, her breathing was completely normal (not loud when at rest or sleeping) and she was not coughing!
November 26, 2007: I didn't want to ever get the call with the pathologist's report. But at 4 p.m., it came. Murphy's surgeon started out by asking how Murphy was doing and we told her she was doing absolutely great. She was very happy to hear that. Then she told us she had the pathology report and said, "The news is not very good." She told us the pathology report had found that Murphy's tumor was not a primary tumor. She had a rare cancer, histiocytic sarcoma, that had spread to her lymph nodes. The surgeon said this kind of rare, aggressive cancer could start anywhere in the body, and it was worse than a high-grade tumor (which she had explained before was a bad tumor). She said that histiocytic sarcoma does not respond to therapies and that the average survival rate was two months. She reported that the complete blood panel and abdominal ultrasound performed prior to surgery were all okay. She asked if Murphy ever coughed up blood because during surgery, she found dried blood in her airway. I told her that I'd never seen Murphy cough up blood. Although she did appear to have something in her mouth sometimes after coughing because she'd move her tongue in an out of her mouth. I thought it may have been mucous, but maybe she was swallowing blood. The doctor recommended that we consult with a veterinary oncologist as soon as Murphy's surgical incision had healed. Fortunately, we had not canceled our original appointment at U.C. Davis oncology for December 3 and when the surgeon heard that she said, "Take it! The sooner you can discuss possible treatment the better." Also, she knew and liked the chief oncologist there.
Two months!?! I am in complete denial at this point. It can't be possible this could be happening to Murphy. I am encouraged, though, by this sentence in the pathologist's report: "These types of tumors are generally not particularly amenable to treatment, however, consultation with a veterinary oncologist may be beneficial." There it is. Our appointment with U.C. Davis will certainly be our saving grace.
All x-rays, blood tests results, ultrasound results, surgical reports and the pathology report were sent to our new home-visiting vet, but he never contacted us. So, we knew for sure that he really did not want to be our vet.
Murphy was doing great and we're going on short walks (although she wants to go longer) and we're pretty much back to our normal routines. Her cough, which we had not heard since her surgery, was slowly coming back.
December 3, 2007: I brought my list of questions with me to U.C. Davis to ask of our oncologist, the very one who our surgeon knew. Our surgeon had already faxed a "Patient Referral" to the oncologist along with Murphy's complete record. The cover sheet to the fax she sent read, in part: "Histopath: high grade histiocytic sarcoma with intralymphatic tumor; presumed metastatic to enlarged nodes. Clients are interested in any options that may prolong the time they have w/Murphy while retaining a good quality of life. Please remove her surgical staples at this visit."
I was very happy to meet our oncologist as he, too, was extremely knowledgeable and had a demeanor that put us all at ease, even though Murphy was doing her usual trembling! The doctor and a veterinary student took Murphy for a physical, chest x-rays, complete blood count and chemistry profile. She had to be sedated to stop her trembling so they could get good chest x-ray images. Her surgical staples were removed as well. All her test results were good, except that the chest-xrays revealed that there was a new small mass that had developed in her right lung and her lymph nodes (hilar lymph nodes) were enlarged, which the doctor said was the reason her cough was still present after surgery. He was very positive, however, when he told us he wanted to put her on chemotherapy (CCNU) and explained how that all would work - three capsules (lomustine, one 40-mg capsule and two 10-mg capsules) administered by us every three weeks, along with an antibiotic (trimethoprim-sulfamethoxazole) to give for 10 days beginning three days after the CCNU pills were given. When I asked him if Murphy were his dog, would he do the chemo, he said, "Yes. It's a no-brainer." He advised that if the chemo were successful, the prognosis for survival could be an additional 6-12 months. He explained that they would do more chest x-rays prior to her third dose of CCNU and that if the drug was working her cough should stop before then. If the drug was not working and her lymph nodes and the new lung mass were bigger, CCNU therapy would be discontinued and we'd have to discuss other treatment options. We were to return in one week for another complete blood count to determine how much bone marrow suppression had occurred as a result of the first CCNU treatment. At U.C. Davis, in clinical trials for histiocytic sarcoma, mast cell tumor, and lymphoma, they were administering Denamarin (a combination of Sam-E and milk thistle) to half of the trial participants to determine whether or not this herbal combination would protect the liver from adverse affects of chemotherapy. He said we could participate, but he could not guarantee that Murphy would not be in the placebo group. He also said we could simply give her Denamarin on our own if we wanted. So I decided I wanted to include that in her therapy as well. We went home with our first dose of CCNU and antibiotic and I was able to obtain Denamarin from a veterinary website.
December 4, 2007: We gave Murphy her first CCNU treatment. Because her oncologist approved it, we continued to give her Rimadyl and we resumed giving her a daily multi-vitamin and a daily glucosamine/chondroitin tablet, both of which she had been taking for years.
December 5, 2007: We noticed that today, Murphy began coughing more often than before when people came to the door, while eating, while resting on the sofa, after grooming herself, and when barking. And now the coughs sounded more like gagging and it happened seven times today.
December 6, 2007: The intensity of her coughing and the frequency had increased and now her breathing sounded like "wheezing" at times. I called the oncologist and he advised this was not normal and recommended we obtain another chest x-ray at our local clinic.
December 7, 2007: We took Murphy to the Specialty Clinic for another chest x-ray. She had five coughing episodes from 1:30 a.m. to 9:40 a.m., but her breathing was somewhat easier while at rest. We received no call back from the radiologist with any results of this chest x-ray and our oncologist was not reachable today.
December 10, 2007: The surgeon at the Specialty Clinic who did Murphy's surgery prescribed a cough medicine (hydrocodone bit/homatropine syrup). I did not give her this medication as I wanted to make sure it was okay with her oncologist first.
 December 11, 2007: Back to U.C. Davis for complete blood count to determine the amount of bone marrow suppression due to chemotherapy. The technician answered my list of questions and advised that we would be notified if there were any abnormalities in the blood test, saying, "No news is good news." It was good news, because we not contacted. I forgot to ask about the loud breathing and panting Murphy was experiencing.
December 11, 2007: Back to U.C. Davis for complete blood count to determine the amount of bone marrow suppression due to chemotherapy. The technician answered my list of questions and advised that we would be notified if there were any abnormalities in the blood test, saying, "No news is good news." It was good news, because we not contacted. I forgot to ask about the loud breathing and panting Murphy was experiencing.
December 12-25, 2007: Murphy's cough persisted and her breathing was back to being loud at rest and while sleeping. Everything else about her, though, was totally back to normal. Our Christmas preparations continued. We took our family Christmas photo with Murphy. Everyone consistently told us she looked absolutely great and, in fact, from December 23 through Christmas day we had lots of people coming and going to celebrate the holiday. Everyone, to a person, could not believe Murphy was sick and one relative, who had lost a dog to lung tumors, told me not to worry at all because he heard Murphy's cough and it was nowhere near as bad as his dog's was and his dog lived for a year with those coughing spells. Murphy was happy, active, opened her Christmas presents, proceeded to tear open her stuffed toys, begged food from everyone, ate her meals, played, went for walks, and had a great time. As a result, my Christmas was wonderful!
December 26, 2007: Back to U.C. Davis for a quick check-up by her oncologist prior to getting her second dose of CCNU. Her discharge papers read, "Murph the Smurf looks great. We are sending her home with her second dose of chemotherapy. We need to see her back in three weeks." The second dose of CCNU was given to Murphy with her evening meal.
December 31, 2007: We were back to taking pretty long walks, and today while passing our friend's house (who has Buddy, Murphy's long-time friend) at about 4 p.m., we were invited inside and ended up staying for dinner. I had taken Murphy home at around 5:30 to give her her dinner and then we drove back to Buddy's house, where we stayed till 9:00 p.m. Murphy's cough had progressed by now to the point where it sounded like a loud combination cough/gag. It's hard to describe but it didn't sound like a dog vomiting, but it sounded more like a human vomiting loudly. Anyway, it frightened our friend's 9-year old son to hear her cough.
January 5, 2008: Murphy coughed immediately after eating her lunch and vomited all her food.
January 9, 2009: Murphy went for nine hours today without coughing once!
January 12, 2008: Murphy went for a long walk today.
January 16, 2008: We went back to U.C. Davis today to get more chest x-rays to determine whether or not the chemotherapy was working and, therefore, whether Murphy would get her third dose of CCNU or not. If the lymph nodes in her chest were still swollen and the mass in her lung had not decreased, she would not be continuing with chemo.
She was so happy this morning and playful. She stole my slipper twice (with lots of wagging going on) before leaving for our appointment. I saw a rainbow on our way to Davis. I thought it was a sign of good luck, that we might finally get some good news. That combined with the fact that she was so happy that morning that she played our little game of stealing my slipper twice! I was so hopeful that there might be a good report that day - for a change. Now I think the rainbow sighting may have been a message of another sort.
When we arrived at the hospital, they took Murphy for her x-rays and again they had to sedate her so she would stop trembling so they could get good images. When the results of the chest x-rays were available, her oncologist called us in to view them. When we walked into the room, he was already there at the computer screen and his first words to us were, "It's worse." I made him repeat that. He showed us how, compared to the chest x-rays they had taken on December 3, a month and a half earlier, her trachea was being compressed by tumors on the lymph nodes surrounding it. The trachea opening was half of what it was on December 3. The doctor said the CCNU did not work and that was the only form of chemotherapy that even had a chance of possibly working. She would not be given her third dose of CCNU, and the only other option now would be to consider radiation therapy. He arranged for us to speak to a radiation oncologist while we were there at the hospital.
The radiation oncologist advised that in all the time he had worked with radiating cancer patients, only two had histiocytic sarcoma. He explained that while these tumors responded well to radiation, in both cases new tumors "popped up" in other locations later. He expressed concern regarding performing radiation on Murphy because of the fact that the area that needed to be radiated was so close to her heart and other lung tissue. He said he would need a CT scan done to determine whether or not she would even be a viable candidate for radiation.
My husband and I decided to schedule the CT scan so the radiation oncologist could make that call, so we took the earliest appointment we could get to bring her back for the CT scan, January 28, 1008.
Murphy did not cough in our presence this entire day, I think due to the fact that she was sedated prior to getting her chest x-ray. It always took her awhile to fully recover from being sedated.
January 19, 2008: Today is two months from the date of surgery - the average survival time from diagnosis of histiocytic sarcoma. Murphy is still alive!
January 22, 2008: Started Murphy on the cough suppressant prescribed earlier for a dry, hacking cough, which was okay'd by her oncologist. By the way, Murphy never once coughed in the presence of any of her doctors. I know because I was either there with her or if they took her away, I asked them when they brought her back. The answer was always no, they had not heard her cough.
January 26, 2008: Stopped cough medicine as it did not work and it made Murphy a little loopy.
January 28, 2008: Murphy goes to U.C. Davis this morning for her CT scan after fasting for 12 hours. They took her away and we waited for seven hours before we got her back. They had to anesthetize her prior to doing the CT scan. When the oncologist was available, he called us in to see the results of the CT scan. He explained that tumors had developed like a cluster of grapes all around her airways (both left and right sides) and that she was not getting very much air. He showed us the images on the computer screen and I have to admit that I really didn't know what I was looking at. All I know was that the doctor did not appear to be very optimistic at this point. Again, he arranged for us to speak to a radiation oncologist about Murphy's candidacy for radiation therapy.
The radiation oncologist advised me that because Murphy did not have much longer to live, they could do the radiation because she would not live long enough to experience any of the negative long-term affects to the organs exposed to radiation, namely, her heart and lung tissue. She would have to be anesthetized every day for the seven days in succession that she would receive radiation therapy. They would then do another CT scan to see how the radiation was working and may continue treatment for more days of anesthesia and radiation.
I decided not to put her through radiation therapy. I could not imagine how traumatized she would be and how she would respond to having to be anesthetized every day for such a long period of time. She always took at least two days to completely recover from anesthesia she had for prior surgeries. I couldn't let that happen every single day.
January 30-31, 2008: Murphy's cough was getting more frequent and she developed a nasal-sounding congestion while breathing at rest. It sounded like her nose was stuffed up and she needed to blow her nose.  The nasal congestion while at rest didn't happen all the time, though.
The nasal congestion while at rest didn't happen all the time, though.
February 4, 2008: Vomited her dinner at 9:00 p.m.
February 5-6, 2008: At this point, I should mention that Murphy's appetite had not dwindled in the least. She was still eating all her meals, snacks, treats, and licking our dinner dishes/pots/pans prior to them going into the dishwasher every night. We were still going on short morning walks and somewhat longer late afternoon walks, but these walks have slowed down considerably and are of a much, much shorter duration than ever before. Her energy level has diminished.
February 7, 2008: I took Murphy for our morning walk, which was about a block and a half from home and back. When we reached our entry path to the front door, Murphy seemed to want to lie down, but couldn't. She kept circling with her knees bent as if trying to lie down, but wasn't able to. I called her and tried to get her to come inside and when she walked up the two steps to the front door, she stumbled off the top step. Didn't fall down, but was still trying to lie down. When I finally got her to come inside the house, she was still walking around the living room in this bent-over position, looking like she wanted to lie down but couldn't. Finally, in an area of the living room where she absolutely never laid down in, she collapsed on the floor and instantly fell asleep. I thought she was dying, so I laid down on the floor right next to her and started praying. After about ten minutes, our son came out of his room, and Murphy woke up, happy, excited to see him, and completely recovered! When my husband got home later and I told him what had happened, we decided it was time to get her evaluated by a veterinarian to determine where in the process she was and to help us prepare for whatever might be coming next.
For the last couple of days, Murphy slept through her normal dinnertime and ate later than usual. Normally, she would let me know when it was mealtime and if I hadn't already begun to prepare her meal, she would continue to bother me until she got fed! She also started to be a little, tiny bit picky about what she would eat. Some of her favorite snacks (namely, apples and bananas) she either wouldn't eat or would eat only if I put peanut butter on the mashed banana. In the mornings, she would only eat her cookies if they were broken up into very small pieces.
I was lying with Murphy on the bed in the evening when my son came in and sat with us. Murphy was lying on her side and he must have noticed how hard she was pumping to breathe. He said to her, "You're really working hard to keep that thing going, aren't you."
February 8, 2008: I didn't want to put Murphy through the trauma of going to a new veterinarian's office and wanted to avoid all the shaking and heavy panting she did when at the vet's. I truly didn't think she could take it anymore. So, my husband researched veterinarians who made housecalls, found one, and made an appointment for him to come to the house on February 13, 2008, to examine Murphy and based on his evaluation of the status of her health, to discuss when it might be time to consider euthanasia.
February 9, 2008: We briefly visited our friend who has Buddy. Our friend noticed how Murphy's abdomen is pumping hard while breathing.
February 10, 2008: We drive Murphy to her favorite walking spot, a place we used to walk to every day - about a ten block walk in one direction, around a very large wooded area, and then back home. It would normally take us about an hour and 20 minutes to do the whole walk. We used to do this every single day. She can't make it there anymore, so we drove her and she actually took a short swim in the creek! Then we walked around the wooded area, met some dog friends, and drove home. It was a great time for all of us.
February 12, 2008: We drove Murphy to the creek area again today and again she went for a quick swim. We met more dog friends and drove home.
February 13, 2008: This morning, before the new home-visiting vet arrived, Murphy was in her favorite spot on the couch watching out the glass doors leading to the backyard when all of a sudden (just like in the old days), she started barking and leaped over the arm of the sofa toward the doors. I opened the door and she saw a cat walking across the top of our fence. She took off after it as if she was two years old! Then about 20 minutes later (I guess the cat was on his return trip), she did the same thing again. I was so encouraged by this behavior. I thought I had my old girl back!
When the vet arrived, my husband had Murphy on leash walking in front of the house. They all came inside together and the vet said when he saw Murphy he was surprised at how good she looked and acted and he wondered why we would be thinking of euthanasia. I told him we only wanted an examination at this point and the vet seemed relieved.
After examining her, the vet told us we were on "overtime" with Murphy (because she had made it a month beyond the average two-month survival period), that her form of cancer was bad, that her lungs sounded very "noisy," and her breathing was labored as evidenced by the fact that she was using her abdominal muscles to push air in and out of her lungs. But otherwise, she looked good. When I asked about the incident when she collapsed in the living room and instantly fell asleep after our morning walk (on February 7), the vet said that we had to remember that because of her condition and the loss of part of her left lung at surgery, it was as if we had a six cylinder car that was running on only three cylinders. We should think of Murphy as running on only three instead of six cylinders now and only take her on very short easy walks. In his opinion, the collapsing was simply from exhaustion. We all agreed to try her on an extended-release bronchodilator medication (Theophylline) to hopefully help her airway open up a bit more to aid in her breathing, along with an expectorant in pill form, since her now horrific cough sometimes produced mucous and getting rid of as much mucous as possible might help the coughing.
Her cough has gotten to the point that when she's lying down and she changes her position, it launches her into a coughing spell. Often, when she jumps up on the sofa, she'll cough, so she jumps back down and lies on the floor. So, Murphy and I are not able to get into our favorite snuggling position on the sofa anymore.
February 14, 2008: I picked up the medications from the pharmacy and at 3 p.m., I administered them (per the doctor's instructions on the label, which I verified with him on the phone). After about three hours, Murphy began experiencing all the possible negative side effects of the bronchodilator medication: agitation, shaking, insomnia, diarrhea, difficulty breathing (and later vomiting). At 11:30 p.m. on February 14, 2008, we took her to the Emergency Clinic. The doctor on duty determined that Murphy had received too much of the bronchodilator and administered a sedative drug (Torbugesic) to her to help calm her agitation. She told us not to give her any more of the bronchodilator (which we were supposed to administer every 12 hours). This Emergency Clinic is also the Specialty Clinic where Murphy underwent surgery to remove the lung tumor back in November of 2007. The doctor who performed that surgery happened to be on duty that night and recognized Murphy. The surgeon commented to the attending doctor that Murphy "looked great." When Murphy was released to us (because the doctor said her heart rate was good), the doctor also told us that Murphy had vomited her entire dinner.
February 15, 2008: We got Murphy home at around 1:30 a.m. I was up all night with her. She couldn't sleep, her breathing was difficult with heavy panting at times, her diarrhea continued, she was restless and seemed uncomfortable. She would sit and just stare into space for long periods of time and if she laid her head down, after a few moments, she'd lift her head back up to about two inches off the ground and keep it there. I thought maybe she was doing this to help her breathe easier. She seemed to be unable to lie on her side. At one point while it was still dark, she went out into the backyard and sat in the middle of the rocks she usually urinated on and with her back to the house, just stared out at the back fence. I watched her for a few minutes, then went out and got her to come back inside. Perhaps it was the medications she was on, but Murphy didn't cough for a very long, long time until at one point, she began a big coughing spell and coughed up mucous that had a pinkish color. She may have slept on and off for maybe two hours maximum (part of the time on the sofa) by the time my husband got up and came out to where we were in the living room at about 7:45 a.m.
I tried to get Murphy to eat something several times during the day and she wouldn't eat anything, not even small pieces of filet mignon left over from our dinner the night before or some thinly sliced roast beef which I had just purchased the day before to help her take her newly-prescribed pills. She just wanted to drink water. I was able to cuddle with her on the floor for about 45 minutes in mid-afternoon, but her behavior really didn't improve the rest of the day until we gave her another dose of a mild sedative the doctor at the Emergency Clinic sent home with us. It allowed her to rest for about two hours beginning at around 4 p.m.
 That day, another entity must have inhabited my body as I made the decision to say goodbye to my soulmate. Why did I decide today? Was it my fear of her death, my fear that she might possibly suffocate? Did I want to just get it over with? Surrendering to the seemingly hopelessness of the situation? I was able to look in her eyes that day and say to her, "I've lost you, haven't I?" I told her she would see "Grandma and Georgie" (my deceased mother and uncle) again. When I said "Georgie," her ears perked and she looked at me, remembering who he was. I hope (but don't remember) that I told her I loved her (as I told her everyday) and didn't know how I could live without her, that she was my heart, my soul, and my life, and thanked her for all the love and joy she brought me. I hope I said these things to her, but I don't remember if I did. I do know that I cut pieces of her hair to keep as precious mementos. I had already made an imprint of her paw in plaster. I did all this with efficiency and not much emotion. I don't know how. How could I? I had already planned it all out in my mind how it should be done. I wanted it to be done at home because she was so afraid of going to the vet and I didn't want her to be scared. I wanted it to happen at the foot of our bed, where she slept for the entire 11 years and 9 months I was privileged to have her with me.
That day, another entity must have inhabited my body as I made the decision to say goodbye to my soulmate. Why did I decide today? Was it my fear of her death, my fear that she might possibly suffocate? Did I want to just get it over with? Surrendering to the seemingly hopelessness of the situation? I was able to look in her eyes that day and say to her, "I've lost you, haven't I?" I told her she would see "Grandma and Georgie" (my deceased mother and uncle) again. When I said "Georgie," her ears perked and she looked at me, remembering who he was. I hope (but don't remember) that I told her I loved her (as I told her everyday) and didn't know how I could live without her, that she was my heart, my soul, and my life, and thanked her for all the love and joy she brought me. I hope I said these things to her, but I don't remember if I did. I do know that I cut pieces of her hair to keep as precious mementos. I had already made an imprint of her paw in plaster. I did all this with efficiency and not much emotion. I don't know how. How could I? I had already planned it all out in my mind how it should be done. I wanted it to be done at home because she was so afraid of going to the vet and I didn't want her to be scared. I wanted it to happen at the foot of our bed, where she slept for the entire 11 years and 9 months I was privileged to have her with me.
Friday February 15, 2008, was the day before the beginning of the President's Day three-day weekend. My husband made the call to the home-visiting vet requesting euthanasia. The vet said he could be here between 7:15 and 7:30 p.m. My husband also called our son who was away for the long weekend because he knew our son would want to be here to say goodbye to Murphy. We waited in numbness. When our son arrived home, we talked and my husband said we didn't have to do it tonight. We could wait and see if Murphy recovered from the medication overdose. Our son agreed. The only thing was that if she did not recover, or got worse, we would have to take her to the Emergency Clinic to have her put to sleep - it couldn't happen at home, like I wanted because of the long weekend and the fact that the home-visiting vet would not come to the house on the weekend. My husband said he didn't want me to be guilt-ridden with the decision, so we could wait. I think I felt pressured now to go through with it because the calls had already been made, our son had returned home, the vet was on his way, and things had been set in motion.
The doorbell rang at 7:15 p.m., and when the vet entered the house, Murphy walked over to greet him, tail wagging. The vet said he didn't want to talk us into making any decision and apologized for the problems with the medications. He said he really only wanted to help and thought the meds would be worth trying. He could sense we were in complete confusion as to what to do. Looking at Murphy's labored breathing, he said, "It's not going to get any better."
I then jumped into emotionless efficiency mode and prepared the foot of our bed for Murphy with a plastic bag over which I placed a thick towel and then a clean sheet. I came back out into the living room where everyone was waiting and said, "Murphy, let's go night-night, sweetie. Let's go to bed, baby-girl." She ran after me into the bedroom and jumped right up on the bed and into her spot. I don't know how I did all this.
She left us while my husband, my son, and I sobbed on her, stroking her, and speaking to her continuously. She was gone by 7:45 p.m. When it was over, the vet said, "About the payment" and after a second or two, I jumped up in my efficient manner and said, "I'll do it," and left my husband and my son with Murphy while I left the room and wrote the check to the vet, which included the cost of cremation.
I wish I hadn't seen the vet place Murphy's sweet, warm, soft, snuggly, love-filled body in the plastic "body bag."
I'm now struggling with feelings of guilt. Should I have waited? Should we have given her another day to try to recover from that medication overdose? Especially knowing how hard it was for her and how long it took her to recover from anesthetics, sedatives, and other medications. Should I have waited? I cannot seem to accept what happened cause;
Murphy never coughed once in the presence of a veterinarian.
She never lost one pound her weight was still the same as it was when she was healthy.
She didn't eat for only one day.
Her vision was good.
Her hearing was good.
She was completely continent.
She had only a little arthritis.
She had so many lipomas (fatty tumors under the skin) that you couldn't count them all. And she had histiocytic sarcoma - the only thing that was wrong with her and that made me feel that her situation was hopeless.
She was too young. Eleven years and nine months old is not old enough to me. I always prayed she'd live to be an old dog. I would have never minded caring for her at age 16. This should have never happened to my sweet baby-girl.
After Murphy was diagnosed with this cancer, I prayed long and hard everyday for a miracle to happen. I wanted the doctors to be wrong. I tried to have faith that it was possible for Murphy to go down in the annals of veterinary medicine as the miracle dog who overcame this impossible cancer. That somehow her miraculous survival would inform veterinarians about this rare form of cancer and that it really wasn't as hopeless as it seemed.
The context of my life now is, "The last time we did this, you were still here. The last time we saw this, you were still here. You would love this, if only you were still here. But, you're not, and I am."
She was my everything and I was hers. Anything I did in my life was made better by her presence. I thank God every night for every second I was blessed with Murphy in my life and all the love and joy she brought me. I thank Murphy every day and every night for that, too.
I want her back.
Written by Vickie Day, who is blessed to be Murphy's mom
I miss you so much, sweetheart

